It has been over a year since I left an OBL to pursue locums. I couldn’t help but think about the process of being involved in OBL development. From the days during the middle of the pandemic visiting the site as it was being built out to spending countless hours marketing, and even doing other random things like making Costco runs for patient snacks, assembling furniture, or creating the clinic intake forms and order sheets. While I was only a minority owner and I ended up moving on, I took a lot of pride in the success of the business and supporting my partner. I had the privilege of helping hire over 15 employees, some of whom remain good friends, and being introduced to the highs and lows of business ownership.
When things took a turn in my business partnership I couldn’t help but feel frustrated. After all this hard work, why is this happening to me? It’s amazing how easy it is to feel defeated at that moment, but in hindsight what an absolute blessing in disguise. This experience taught me a few key things:
- I enjoy helping others through entrepreneurship.
- Patience is truly a virtue.
- Culture matters.
I previously documented, in extensive and colorful detail, my OBL experience and what led to my exit. I subsequently had to remove this heartfelt, and authentic material after being accosted by a lawyer (greetings, friend). Long story short, I was not happy with the direction of the business nor my prospects for future growth, despite what was a growing and robust practice in which I took a lot of pride. Simultaneously, I realized I was selling myself short. I was capable of so much more.
At the end of the day, an argument about the legality of my content tends to be a petty he-said/she-said time, money, and energy suck which gets away from my true mission which is to promote a future of physician entrepreneurship. I no longer live my life worrying about “them,” but before reaching this realization I needed a literal escape. My wife was set to move away for fellowship in a location we had no intention of settling in long-term. I should probably do an entire post on long-distance relationships and the Guantanamo-Bay-like cruelty of academic vascular surgery (talk about a culture problem). So I made a move, quite randomly, to clear my mind and just try something new while I was in a place in my life with the bandwidth to do so.
I went to what seemed like the North Pole, committing to three months of locums in Minnesota while I would search for a new OBL opportunity closer to home. I knew nothing about locums, or the Upper Midwest other than the movie “Fargo.”
Two things happened at the end of 2021. First, I interviewed at 5 different OBLs in the Southeast and came to the same realization each time that I was tired of making other people rich when I’m fully capable of running my own practice, and two, I enjoyed working locums with a great cast of characters up north. I decided to extend my contract another 12 months.
Full-time hospital work was too much for me to stomach, so I structured my schedule to what amounted to a ⅔ FTE position and rounded out the remaining weeks by directly contracting with OBLs. Before you knew it, I had a busy schedule practicing on my terms, and making a good living. As I look back on this experience and the rollercoaster ride that was 2021 and 2022, I thank my lucky stars.
Working locums in Minnesota was a game changer for me. I got to meet three of the best colleagues I have ever worked with in my life: Two senior IRs who have been around the block and a PA of my vintage, all of whom are humble, and supportive and were looking to work with someone interested in supporting a growing clinical practice. Being forced to deal with the usual hospital work and rekindle dormant skills in the form of VTE intervention, portal hypertension work, and bleeders of all varieties forced me to adapt. I was lucky to introduce prostate artery embolization to two willing colleagues who were interested in improving their skills. I approached this position doing what I could to be as helpful as possible and at the same time working as much as I could safely handle to both maximize my revenue potential and continue to improve my skills as an IR. I ended up taking 32 weeks of call over a year and pushed myself to extreme limits working some ridiculous hours, doing some insane cases, and making the most of my IR training. The year was one of significant personal, professional and financial growth.

I was privileged to work with a fantastic group of nurses, technologists, sonographers, and patient transporters who were genuinely interested in helping their physicians take the best care of patients possible. Of course, despite the great camaraderie and support, my initial perception of hospital-based IR was more than just a biased representation based on my first job out of training. It was clear that the challenges I faced in my first two years in practice are prevalent in any hospital. It took me one particularly rough day to put hospital life in context and to be angry enough to produce what is likely the highlight of my career as a writer. The struggles IRs face reflect a microcosm of the healthcare system in which we practice.
Everyone Is Replaceable
Whenever you spend a lot of time in someone’s home, it’s not too hard to feel like a part of the family. Having spent 2-3 weeks a month at this particular hospital, it essentially felt like home. And while for the most part that was a positive experience, families are never perfect and before you know it the imperfections become quite obvious.
My experience working in Minnesota was the first time I was exposed to a model of direct healthcare system employment. In this particular large organization, radiologists, including IRs, were directly employed and had at least three layers of administration between them and the C-suite. While this was an incredibly progressive IR practice (“100% IR,” rounding service and weekly clinic), the group was still lumped into the financial division of radiology. Larger decisions concerning the department included IR which invited the standard RVU wars which I have spoken about in the past. As a developing clinical service with historical trash collection expectations among referring physicians in this tertiary care center, the section was not immune to a high volume of mundane procedures. As such, IR RVUs did not come anywhere close to the RVUs of diagnostic radiologists. While this historically has not been an issue as the division chief took the position six years ago with a handshake agreement between him and the administration at that time that his focus should be on growing the section and supporting the needs of the hospital and larger healthcare system. Being an excellent and ambitious IR, he grew the section nicely, eventually bringing on a very experienced IR several years ago. The section eventually grew to three, but unfortunately, their young new hire did not work out for a variety of reasons prompting the division to seek locums help until a new fellowship graduate would start in the Fall of 2022.
Probably for the first time in my life, I found myself in a division where I was aligned with the goals of both of my partners. Over time I got to know them both well and they became great friends and colleagues. During this time I also witnessed the complete lack of control we as physicians have within healthcare systems where we are employees.
About several months into my hospital tenure, the division chief got notice that a new administrative vice-president would be in charge of radiology system-wide. Shortly thereafter a radiology department meeting took place where non-physician leadership proposed a plan where IR absorbs all procedures, including things like LPs, arthrograms, paracentesis and barium studies. The same plan included IRs helping with diagnostic reads as the current diagnostic radiologists were stretched thin with increasing volumes and an inability to hire in the current market. As you would expect, that did not sit well with the two permanent IRs. They both took this job to practice 100% IR in an environment that values their contributions.
At this point, my colleagues came to realize that I was somebody who enjoyed speaking (I gave a couple of hospital grand rounds) and writing (pretty sure they heard about the blog), so they asked if I could help them out. I wasn’t sure how exactly, but I ended up crafting the following letter as their ghostwriter with names and locations removed:
To Whom It May Concern,
In the short time since we have been working at [this system] as interventional radiologists, we have seen significant growth in our division. Before 2016, many image-guided interventions which are critical to the functioning of a tertiary/level I trauma center setting such as ours were very fragmented. Since our arrival, we have been able to streamline these services into our division and become a trusted resource for many of our colleagues in this institution.
As we look to [insert cute project name for hospital expansion] and the continued expansion of our healthcare system, we have reflected upon our values and have created an enhanced vision for ourselves as we expand existing service lines which can play a crucial role in supporting the health of our community including venous thromboembolism interventions, interventional oncology, women’s and men’s health interventions and limb salvage. Similar to surgical and medical subspecialties, interventional radiology is capable of generating referrals through marketing efforts. Together with our talented colleagues, we can continue to grow a robust program where we can practice interventional radiology at the highest level possible to better support our healthcare system and improve the lives of patients in our region.
In order to do this, we require buy-in from key stakeholders in administration so we can make the infrastructural and personnel investments that can help bring our vision to life. We would like to bring on additional physicians and advanced practice providers to grow our division. Through daily longitudinal clinics, inpatient rounding services, and improved outreach to other physicians and advanced practice providers in our system, we hope to use our passion for image-guided therapies to improve the level of service we provide for both patients and referring colleagues.
The value of a clinically oriented interventional radiology division to a large healthcare system cannot be overstated. We provide an essential service to the hospital ranging from routine procedures such as central venous access to advanced life-saving services such as embolotherapy and pulmonary arterial interventions. Without our presence, the smooth functioning of a large hospital with many surgical and medical specialists who depend on us to care for their patients is not possible. Unfortunately, our value to the healthcare system and the patients it serves is not readily reflected in common financial metrics used to assess radiology production as procedures most commonly associated with interventional radiology have low relative value unit designation, yet are essential for patient care. What is not readily apparent is our potential to generate even more revenue when we have the infrastructure to build clinical programs which allow us to break the mold of our traditional role as “proceduralists.” We feel confident that any of our referring physicians and advanced practice providers would convey their gratitude and appreciation for the level of service we provide and would gladly support our goal to expand our services.
We hope you share our vision to improve our existing service and create new service lines to better support patients and bring new patients into the healthcare system. At the end of the day, when clinical interventional radiology services can thrive, patients win and that is what matters the most.
Kindly,
[IR Divison Chief and Trusted Partner]
I was proud of this letter, but sadly in the back of my head, I had a feeling that the new administrative vice-president on the other end would not care. In typical hospital administration fashion, things dragged on without a clear resolution. Lots of emails were sent back and forth with plenty of mentions of “circling back” and maybe taking ‘things offline to discuss further,” but to no clear or expedient resolution. Based on what I learned about the new administrative vice president and their tendency to make unilateral decisions driven solely by Excel spreadsheets and not taking into account actual human beings, I knew my future in this setting was bleak.
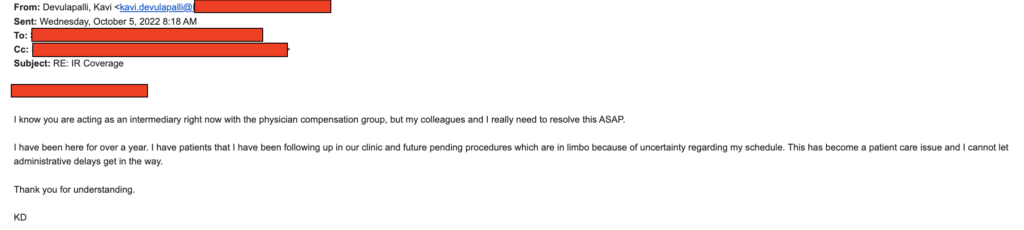
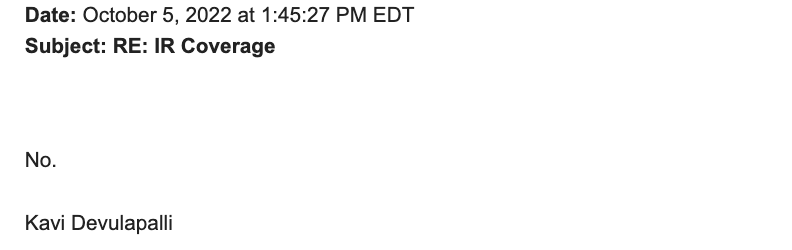
This individual decided to terminate my locums agency contract immediately after the new IR hire started. This administrator never met me or communicated with me in any fashion before doing so. After the division chief made it clear that he and the other IR would like to retain my services, only then did the administrator engage me in conversations to potentially reach a new independent contractor agreement directly with the healthcare system. We ended up having detailed discussions at the last minute prior to my scheduled departure about how I can continue to contribute to the department for up to a week a month, but ultimately the administration’s counteroffer to my request was so insulting that I decided to pull the cord and move on. I’ve dealt with enough healthcare industry terrorists in my life. Let’s just say that the offered pay was pro-rated less than what the employed IRs were making. As much as I love the team where I was working, I’m not running a charity. Check out the email screen shots for your entertainment.

And just like that my time in the cold white North came to an end. It ended on a positive note with some wonderful gifts and acknowledgments from the staff and my colleagues. Perhaps in an alternative universe where I enjoyed being an abused W2 wage earner for faceless MBAs clocking 40-hour workweeks remotely and making more money than I did when I first started my career as an attending IR, I’d consider formal employment, but my time was up and I was meant to move on to other things.
The experience taught me that no one is truly protected from the greater forces of healthcare finances and political headwinds in any institution at any given time. There are luminaries in our own field who were forced out of positions and sent packing with their tails tucked between their legs looking for new opportunities. For this crafty Monkey, I did what I know best, which is to adapt and ramp up work with existing clients, establish relationships with new OBL clients, and bring on a new hospital client through some wonderful industry contacts (thank you, Chris). The beauty of our skillset in IR is we can not only always keep the lights on, but we can thrive no matter the circumstances. Ever since this event in Minnesota, I’ve had another contract fall through on short notice forcing me to call an audible. As they say, freedom isn’t free. Nevertheless, diversification of income streams is essential and allows me to sleep well at night.
It turns out though that the challenges we face as physicians in healthcare are not that different from some of our trusted non-physician colleagues. During my time in Minnesota, I experienced the largest nursing strike in US history. I was so moved by their request for basic respect from institutions making billions of dollars, I took some time out of my day on a pleasant summer day to go marching with them between cases.
In healthcare, as is similar to any industry where one does not control their own destiny, everyone is replaceable. It does not matter how good you are or how honest you are. If your presence does not fit within the agenda of anyone who controls you as an asset, you are simply expendable.
As physicians, we are smart, hard-working, and largely honest individuals who mean well. Why in the world do we continue to feed into this system where we are being used and abused by people who do not share our interests? Why do we take jobs with organizations that could not care less about our well-being or our moral obligation to patients? Better yet, why do we gaslight other physicians into believing that not making a particular situation work is somehow the fault of the physician who is perhaps “not a team player.” Frankly, I’m tired of bending over backward for individuals, groups, and institutions who treat us like dirt. I’d honestly rather be unemployed than work for someone I do not trust. Frankly, I’m done working for anyone other than myself. I’d encourage more of you to act similarly. Position yourselves to make them need you, not the other way around. Perhaps if we all operated in this fashion then real change could be had.
My existence as a locums physician continues with new lessons learned and new wonderful experiences to share. Look for an update on “Locums Life” to hit this blog soon, with a summary of actionable content based on my adventures in this line of work. Until then, thanks for taking the time to read about my experiences. Looking forward to bringing you more content as I live it.

“No.”
straight gangster
Started the school believing Rosseau was right.
Leaving the hypocritical cesspool that is “modern medicine”, believing that Hobbes was right.
I don’t give a flying damn about the higher ups that “they don’t need me” and telling me indirectly that I am expendable. If I’d be just another body bag, at least I’d find other fields where I could get more money.
I’m thinking investment banking. Money makes the world go around. The only way to make your ideals true is with influence and money; you will not have these in short supply outside of medicine.
Human compassion has always been taken for granted. I went to the field good intentions. Now, I leave it with only a bitter taste. If I am expendable, I will tell the others that in the white coat of lies that they will eventually become expendables. The propaganda of “perfect doctors” that seems to operate on pure hope and compassion that is willing to work for free for their betterment of patients as the “minimum standards” is disgusting.
At least, in the financial sector at least, there is no pretense or hiding the fact that profit is king. Perhaps that white coat is only a signifier that the profession will only tell white lies to yourselves that to think of one’s own well-being is “evil.” If that is “evil”, so I will be.